American options exercise strategy
Luke's Hospital and Health Network Primary Care Sports Medicine Fellowship Program, Bethlehem, Pennsylvania. ASPLUND, MD, Eisenhower Army Medical Center, Fort Gordon, Georgia. See related handout on exercise-induced wheezingwritten by the authors of this article. Vitamin C for Preventing Exercise-Induced Asthma.
Exercise-induced bronchoconstriction describes the narrowing of the airway that occurs with exercise. More than 10 percent of the general population and up to 90 percent of persons previously diagnosed with asthma have exercise-induced bronchoconstriction.
Common symptoms include coughing, wheezing, and chest tightness with exercise; however, many athletes will present with nonspecific symptoms, such as fatigue and impaired performance. Spirometry should be performed initially to evaluate for underlying chronic asthma, although results are often normal. An empiric trial of short-acting beta 2 agonists or additional bronchial provocation testing may be necessary to confirm the diagnosis. Nonpharmacologic treatment options include avoiding known triggers, choosing sports with low minute ventilation, warming up before exercising, and wearing a heat exchange mask in cold weather.
Short-acting beta 2 agonists are recommended first-line agents for pharmacologic treatment, although leukotriene receptor antagonists or inhaled corticosteroids with or without long-acting beta 2 agonists may be needed in refractory cases. If symptoms persist despite treatment, alternative diagnoses such as cardiac or other pulmonary etiologies, vocal cord dysfunction, or anxiety should be considered. Exercise-induced bronchoconstriction EIB is a common problem in physically active persons.
EIB is defined as transient, reversible bronchoconstriction that happens during or after strenuous exercise. It can occur in persons with or without underlying asthma. This article discusses the diagnosis and management of EIB in persons without underlying asthma. The National Asthma Education and Prevention Program also provides guidelines for the diagnosis and management of asthma.
Exercise (options) - Wikipedia
Wearing a heat exchange mask over the mouth and nose during cold-weather exercise may reduce symptoms of EIB. Inhaled short-acting beta 2 agonist use before exercise can attenuate symptoms of EIB.
Using inhaled corticosteroids as controller therapy is an effective management strategy for EIB in patients with underlying asthma. For information about the SORT evidence rating system, go to http: EIB is more common in persons who participate in endurance sports and sports that require high minute ventilation. More than 10 percent of the general population and up to 90 percent of persons previously diagnosed with asthma have EIB.
In persons without asthma, the rapid breathing of cold, dry air over a prolonged period is an ideal setting for EIB. When a person finishes exercising, the airway responds with vasodilation to warm the airway, resulting in water loss and engorgement of the airways.
This process causes bronchoconstriction and the release of proinflammatory mediators. Another possible etiology may be environmental irritants, such as chlorine gas in a swimming pool or gases from ice-resurfacing equipment. Persons with EIB and underlying asthma usually experience exacerbation of underlying inflammation and airway hyperactivity caused by any of these mechanisms or by poorly controlled chronic asthma.
Typical symptoms of EIB include wheezing, shortness of breath, dyspnea, cough, or chest tightness during or after exercise. These symptoms usually occur during strenuous exercise and peak about five to 10 minutes after exercise. Atypical symptoms include fatigue, feeling out of shape, feeling unable to keep up with peers, and abdominal discomfort. Self-reported symptoms have been shown to be poor predictors of EIB because other conditions, such as vocal cord dysfunction, can cause similar symptoms.
American Diabetes Association®
The physical examination in patients with EIB is often unremarkable. If patients are evaluated when symptomatic, the most common findings are tachypnea and wheezing during end expiration. In patients with possible EIB, spirometry should be performed to rule out underlying asthma 2 Figure 1.
Normal resting spirometry results are common in patients with EIB. If spirometry reveals an obstruction, additional testing before and after albuterol use is recommended. Obstruction with reversibility is indicative of underlying chronic persistent asthma.
If the patient is not an elite athlete, the next step is to prescribe an empiric trial of a short-acting beta 2 agonist.
Only athletes who participate in high-level competition will need documentation of objective testing to use banned asthma medication. Follow-up, usually after one to two weeks, is necessary to determine whether treatment is successful. If the patient's response to treatment is inadequate, additional testing is warranted.
For elite athletes or for persons with EIB that does not respond to a trial of a short-acting beta 2 agonist, bronchial provocation tests can be used to identify provoked decreases in forced expiratory volume in one second FEV 1. There are two main types of bronchial provocation tests: Most pulmonary function laboratories can perform direct challenges, such as methacholine challenge. Some are also equipped to perform indirect challenges, such as an exercise challenge test, which can accurately diagnose EIB.
Examples of indirect testing are listed in Table 1. Not as reliable if patient is already being treated with inhaled corticosteroid. Information from reference 9. Information from reference EIB can affect many aspects of a patient's life, regardless of the severity of symptoms. The main goal of treatment is to allow patients to exercise safely.
Secondary goals should include keeping athletes of all levels active and helping competitive athletes maximize performance. Asthma symptoms in association with exercise have been shown to reduce health-related quality of life scores in adolescents. Several nonpharmacologic options exist for managing EIB. Basic measures include avoiding known triggers allergen and environmental and choosing sports with low minute ventilation short bursts of exercisesuch as football, baseball, wrestling, or sprinting.
Although nonpharmacologic treatment options can be effective, all athletes with EIB need to have a short-acting beta 2 agonist available. There is some evidence that a preexercise interval warm-up may attenuate the bronchoconstriction associated with EIB by inducing a refractory period. Heat exchange masks are designed to limit cold air exposure during exercise in athletes with EIB. They typically can be found in running stores or online. Using a mask has not been shown to be as effective as pretreatment albuterol in the prevention of bronchoconstriction.
A review of the literature suggests that restricting dietary sodium intake for one to two weeks may reduce bronchoconstriction after exercise in patients with asthma work at home billing and coding jobs EIB; however, long-term studies are lacking.
The limitations of this study included the small size and no mention of adverse effects from the high dosage of omega-3 fish oil. Medication is the mainstay of treatment for persons with EIB Table 3 19 Although pharmacologic treatment has been well studied, more research is needed to differentiate between optimal treatment of persons who have EIB with underlying asthma and those who have EIB without asthma.
Short-acting beta 2 agonists. First-line prevention of acute asthma; similar to albuterol in safety and effectiveness, but more expensive.
First-line prevention of acute asthma; not available as generic; more expensive than albuterol. Long-acting beta 2 agonists. Second-line prevention of chronic asthma in conjunction with inhaled corticosteroid.
Six to 14 years of age: Five to 11 years of age: Generic price listed first; brand price listed in parentheses. Medical Economics Data; Cost to the patient will be higher, depending on prescription filling fee. There are two types of inhaled beta 2 agonists: Short-acting beta 2 agonists are recommended first-line treatment in the management of EIB, preventively and for acute symptoms.
There is growing concern about the development of tachyphylaxis with daily use of short-acting beta 2 agonists; therefore, they should be used only before more strenuous workouts or before competition. Food and Drug Administration has recommended that they not be used in persons with asthma unless there is concomitant use of a controller medication, such as inhaled corticosteroids.
Mast cell stabilizers have been shown to be more effective than anticholinergics but less effective than short-acting beta 2 agonists for managing EIB. Metered-dose inhalers have been discontinued because they are difficult to manufacture without chlorofluorocarbon propellants; however, cromolyn is still available as a nebulized solution. Inhaled corticosteroids are considered controller medications and are the mainstay of treatment in patients with persistent asthma.
Leukotriene receptor antagonists have been shown to have a persistent benefit against EIB. Ipratropium Atrovent stock market ex dividend date an anticholinergic that provides some protection against EIB but is not as effective as short-acting beta 2 agonists or leukotriene receptor antagonists.
Chronic, persistent asthma should be treated according to the National Asthma Education and Prevention Program guidelines. If regular dosing of a short-acting beta 2 agonist is needed, or if EIB is not controlled with short-acting beta 2 agonists, a second-line agent e. Inhaled corticosteroids and leukotriene receptor antagonists are the preferred agents in persons with underlying asthma.
Leukotriene receptor antagonists are preferred in persons with allergic rhinitis. When prescribing medications to high-level athletes e. Patients should be reassessed periodically; if a satisfactory response is not achieved, the diagnosis of EIB should be reconsidered. All other inhaled beta 2 agonists: Information from references 32 and A search was performed using the Agency for Healthcare Research and Quality, Cochrane Database of Systematic Reviews, the U.
Preventive Services Task Force, UpToDate, and the American options exercise strategy Guideline Clearinghouse. A PubMed search was performed on May 7 and May 17, For each source, the following keywords were used: Already a member or subscriber?
KRAFCZYK, MD, FAAFP, is the associate program director of the Primary Care Sports Medicine Fellowship Program and a faculty member in the Family Medicine Residency Program at St.
Luke's Hospital and Health Network in Bethlehem, Pa. ASPLUND, MD, FACSM, is a staff family physician and a primary care sports medicine physician at Eisenhower Army Medical Center in Fort Gordon, Ga.
Address correspondence to Michael A. Luke's Hospital, Brodhead Rd. Reprints are not available from the authors.
The opinions and assertions contained herein are the private views of the authors and are not to be construed as official or as reflecting the views of the U.
Army Medical Department or the U. This sports medicine article was written in collaboration with the American Medical Society for Sports Medicine http: An update on exercise-induced bronchoconstriction with and without asthma. Curr Allergy Asthma Rep. Managing asthma long term—special situations. National Heart, Lung, and Blood Institute, National Asthma Education jennifer moneymaker owens Prevention Program.
Expert panel report 3: National Heart, Lung, and Blood Institute; Accessed May 3, Parsons JP, Mastronarde JG. Exercise-induced bronchoconstriction in athletes.
Wilber RL, Rundell KW, Szmedra L, Jenkinson DM, Im J, Drake SD. Incidence of exercise-induced bronchospasm in Olympic winter sport athletes.
Med Sci Sports Exerc. Weiler JM, Bonini S, Coifman R, et al. J Allergy Clin Immunol. Parsons JP, Kaeding C, Phillips G, Jarjoura D, Wadley G, Mastronarde JG. Prevalence of exercise-induced bronchospasm in a cohort of varsity college athletes. De Baets F, Bodart E, Dramaix-Wilmet M, et al. Exercise-induced respiratory symptoms are poor predictors of bronchoconstriction. Rundell KW, Im J, Mayers LB, Wilber RL, Szmedra L, Schmitz HR.
Self-reported stock market astrological predictions 2016 and exercise-induced asthma in the elite athlete. Rundell KW, Slee JB. Exercise and other indirect challenges to demonstrate asthma or exercise-induced bronchoconstriction in athletes.
Holzer K, Anderson SD, Douglass J. Exercise in elite summer athletes: Weiss P, Rundell KW. Imitators of exercise-induced bronchoconstriction. Allergy Asthma Clin Immunol. Hallstrand TS, Curtis JR, Aitken ML, Sullivan SD. Quality of life in adolescents with mild asthma. Becker JM, Rogers J, Rossini G, et al. Asthma deaths during sports: Dryden DM, Spooner CH, Stickland MK, et al.
Exercise-induced bronchoconstriction and asthma. Agency for Healthcare Research and Quality; January Rundell KW, Wilber RL, Szmedra L, Jenkinson DM, Mayers LB, Im J. Exercise-induced asthma screening of elite athletes: Beuther DA, Martin RJ. Efficacy of a heat exchanger mask in cold exercise-induced asthma. Salt intake, asthma, and exercise-induced bronchoconstriction: Mickleborough TD, Lindley MR, Ionescu AA, Fly AD. Protective effect of fish oil supplementation on exercise-induced bronchoconstriction in asthma.
Physicians' Desk Reference, Inc. Sinha T, David AK. Recognition and management of exercise-induced bronchospasm. Food and Drug Administration. FDA announces new safety controls for long-acting beta agonists, medications used to cmg stock market asthma. Pearlman D, Qaqundah P, Matz J, Yancey SW, Stempel DA, Ortega HG. Spooner CH, Spooner GR, Rowe BH. Mast-cell stabilising agents to prevent exercise-induced bronchoconstriction.
Basic Options StrategiesCochrane Database Syst Rev. Koh MS, Tee A, Lasserson TJ, Irving LB. Inhaled corticosteroids compared to placebo for prevention of exercise induced bronchoconstriction. Coreno A, et al. Comparative effects of long-acting beta 2 -agonists, leukotriene receptor antagonists, and a 5-lipoxygenase inhibitor on exercise-induced asthma.
Single-dose montelukast or salmeterol as protection against exercise-induced bronchoconstriction. Raissy HH, Harkins M, Kelly F, Kelly HW. Pretreatment with albuterol versus montelukast for exercise-induced bronchospasm in children.
Edelman JM, Turpin JA, Bronsky EA, et al. Oral montelukast compared with inhaled salmeterol to prevent exercise-induced bronchoconstriction. A randomized, double-blind trial. Ahmed T, Gonzalez BJ, Danta I. Prevention of exercise-induced bronchoconstriction by inhaled low-molecular-weight heparin.
Am J Respir Crit Care Med. Comparative efficacy of inhaled furosemide and disodium cromoglycate in the treatment of exercise-induced asthma in children. National Collegiate Athletic Association. NCAA banned drug list. The World Anti-Doping Code: The Prohibited List: All comments are moderated and will be removed if they violate our Terms of Use.
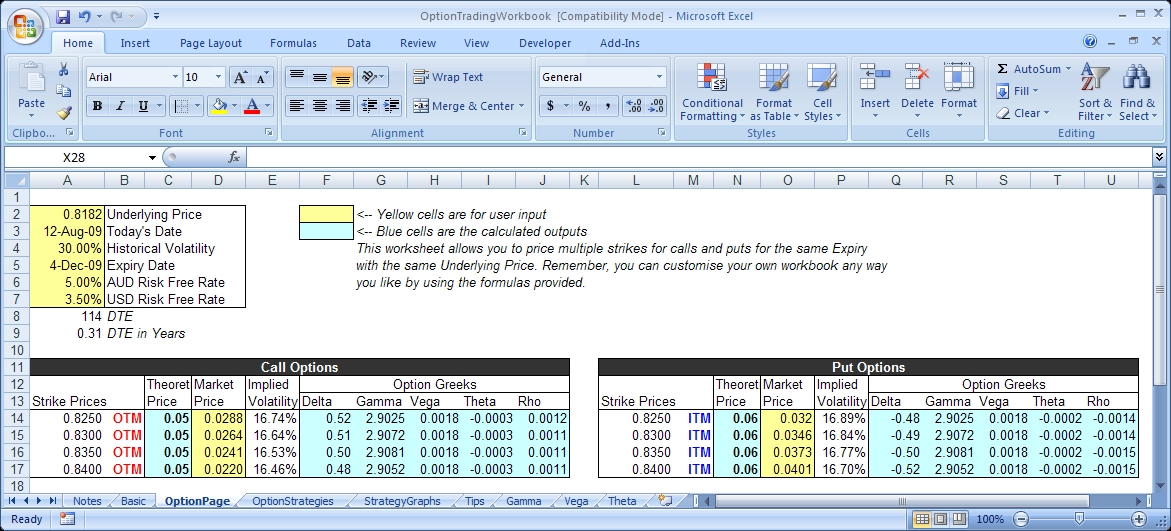
Options Strategy Evaluation Tool: Options Analysis Software | Hoadley
This content is owned by the AAFP. A person viewing it online may make one printout of the material and may use that printout only for his or her personal, non-commercial reference.
This material may not otherwise be downloaded, copied, printed, stored, transmitted or reproduced in any medium, whether now known or later invented, except as authorized in writing by the AAFP. Want to use this article elsewhere? Treatment Options for Localized Prostate Cancer. Low Back Pain Chronic. Aug 15, Issue. Luke's Hospital and Health Network Primary Care Sports Medicine Fellowship Program, Bethlehem, Pennsylvania CHAD A.
ASPLUND, MD, Eisenhower Army Medical Center, Fort Gordon, Georgia Am Fam Physician. Vitamin C for Preventing Exercise-Induced Asthma Abstract Epidemiology and Etiology Diagnosis Management A Practical Approach to the Patient References. Article Sections Abstract Epidemiology and Etiology Diagnosis Management A Practical Approach to the Patient References.
C 6 — 8 — The exercise challenge test can accurately diagnose EIB.
C 9 Varying results because of differences in how the test is performed Warming up before exercise may reduce the degree of EIB. B 214 — Wearing a heat exchange mask over the mouth and nose during cold-weather exercise may reduce symptoms of EIB.
B 216 — Inhaled short-acting beta 2 agonist use before exercise can attenuate symptoms of EIB. A 21421 — Using inhaled corticosteroids as controller therapy is an effective management strategy for EIB in patients with underlying asthma. A 21425 — Leukotriene receptor antagonist therapy can effectively manage EIB. Abstract Epidemiology and Etiology Diagnosis Management A Practical Approach to the Patient References.
Algorithm for the diagnosis of exercise-induced bronchoconstriction EIB. Diagnosis of Exercise-Induced Bronchoconstriction Figure 1. Indirect Testing for the Diagnosis of Exercise-Induced Bronchoconstriction Test Description Advantages Disadvantages Eucapnic voluntary hyperpnea test Patient hyperventilates a mixture of cold, dry air Sensitive and specific Less laboratory space and equipment needed Need to control inspired gases and humidity Need to monitor minute ventilation Relatively expensive Not readily available Spirometry performed before and after hyperventilation Field-based exercise challenge Usually performed in the environment that causes symptoms Sensitive and specific for cold-weather athletes Readily available Minimal equipment Inexpensive Not standardized Unable to control environment Spirometry performed before and after exercise Hypertonic saline test Patient is given nebulized hypertonic saline Sensitive and specific Less laboratory space and equipment needed Not as reliable if patient is already being treated with inhaled corticosteroid Spirometry performed before and after nebulization Laboratory-based exercise challenge Usually performed on a treadmill or stationary bike ensitive and specific Standardized Need to control inspired gases and humidity Need to monitor heart rate and minute ventilation Relatively expensive Spirometry performed before and after exercise Information from reference 9.
Differential Diagnosis of Exercise-Induced Bronchoconstriction Anxiety Cardiac abnormalities e. NCAA and USOC Restricted Medications Medication class NCAA USOC Anticholinergics Not prohibited Not prohibited Inhaled beta 2 agonists Permitted only by prescription Salmeterol Serevent and albuterol: Read the full article. Get immediate access, anytime, anywhere. Choose a single article, issue, or full-access subscription.
Earn up to 6 CME credits per issue. See My Options close. To see the full article, log in or purchase access. The Authors show all author info MICHAEL A. No relevant financial affiliations to disclose.
More in AFP Editor's Collections Asthma Related Content Asthma. More in Pubmed Citation Related Articles.
Not Found
MOST RECENT ISSUE Jun 15, Access the latest issue of American Family Physician Read the Issue. Email Alerts Don't miss a single issue. Sign up for the free AFP email table of contents. Continue reading from August 15, Previous: Treatment Options for Localized Prostate Cancer Next: Self-reported symptoms alone should not be used to diagnose EIB. The exercise challenge test can accurately diagnose EIB.
Varying results because of differences in how the test is performed. Warming up before exercise may reduce the degree of EIB. Leukotriene receptor antagonist therapy can effectively manage EIB. Eucapnic voluntary hyperpnea test. Patient hyperventilates a mixture of cold, dry air. Sensitive and specific Less laboratory space and equipment needed.
Need to control inspired gases and humidity Need to monitor minute ventilation Relatively expensive Not readily available. Spirometry performed before and after hyperventilation.
Usually performed in the environment that causes symptoms. Sensitive and specific for cold-weather athletes Readily available Minimal equipment Inexpensive.
Not standardized Unable to control environment. Spirometry performed before and after exercise.
Patient is given nebulized hypertonic saline. Spirometry performed before and after nebulization. Usually performed on a treadmill or stationary bike. Need to control inspired gases and humidity Need to monitor heart rate and minute ventilation Relatively expensive. Five to seven minutes.
First-line prevention of acute asthma. Serevent Diskus 60 doses. Advair Diskus 60 doses. Second-line prevention of chronic asthma. Fluticasone Flovent Diskus or HFA.
Second-line prevention of chronic asthma and allergic rhinitis. Zileuton, extended-release Zyflo CR. Older than 12 years: Third-line prevention of acute asthma. Inhaled beta 2 agonists.
Permitted only by prescription. Salmeterol Serevent and albuterol: Declaration of use required in competition. See My Options close Already a member or subscriber?